
Inositol for Women: How Vitamin B8 Supports Women’s Health Before & After Menopause
If you want steadier energy, more regular rhythms, and a
By Jake Crossman (CNC-NASM), Nutrition Specialist; Holistic Health Coach; Managing Partner, USA Medical
Last updated: February 14, 2026
If you’ve ever had an stress-related stomach right before a big meeting or after a long week, you’re not imagining things—your digestive system and nervous system are tightly connected. That connection is why “belly tension,” irregular bathroom patterns, and sensitivity can flare when life feels noisy. Two non-intoxicating cannabinoids people often explore for everyday wellness are CBD and CBG, especially when they want a calmer, steadier day-to-day digestive experience.
Here’s what we’ll cover so you can skim to what matters most:
Digestive symptoms can be physical and responsive to emotion at the same time. That doesn’t make them “in your head.” It means your body is doing what bodies do: integrating signals from the brain, nerves, immune system, and intestines. People often describe this as changes in motility (how quickly food moves), sensitivity, and the intensity of sensations.
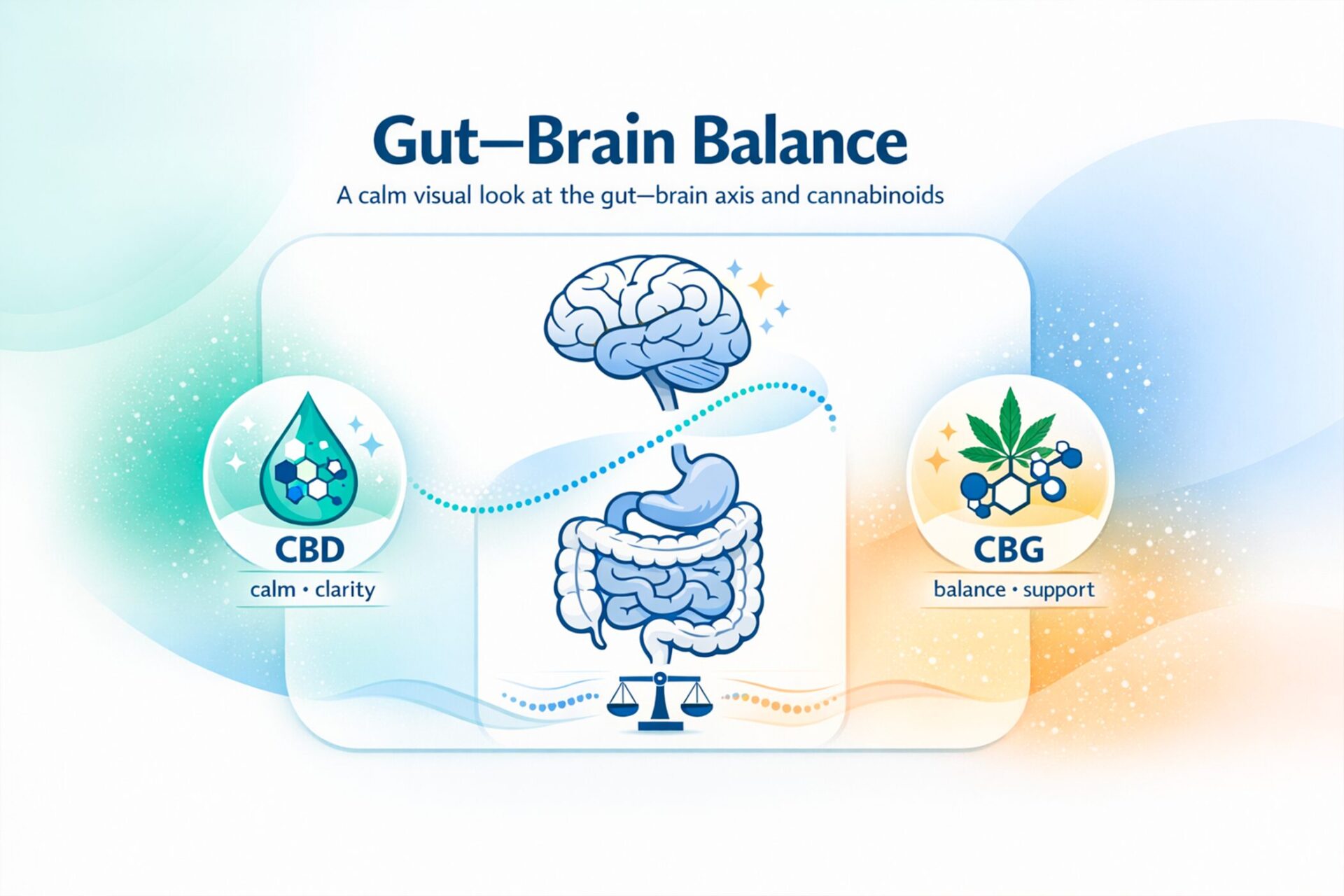
One helpful way to understand this is the gut-brain axis, the communication network linking your brain and your GI tract through nerves and chemical messengers. In conditions like IBS, reputable medical references describe how stress can make intestinal nerves more reactive and the gut more sensitive.
This is also why “settling” strategies sometimes help: if your stress response eases, the gut may feel less reactive. For many people, that’s the doorway to better digestive comfort, even when diet hasn’t changed much.
Some symptom clusters are common enough to have a name, like irritable bowel syndrome, typically involving recurrent abdominal pain plus changes in bowel habits (constipation, diarrhea, or both), often with bloating or a sense of incomplete emptying.
IBS is one example of a “disorder of gut–brain interaction,” where how the gut senses and processes signals can be part of the story. That doesn’t mean cannabis products are a proven treatment; it means stress, sensitivity, and coping tools matter, and it’s reasonable to talk with a clinician when patterns persist.
Takeaway: Stress can amplify gut sensations through real nerve-and-hormone pathways, and recognizing that connection helps you choose smarter, safer tools.
CBD is widely used in wellness routines when someone’s digestive discomfort seems connected to tension, overstimulation, or trouble winding down. The logic is simple: if you can calm the stress response, the gut may feel less “on edge” day to day.
When people say CBD feels “settling,” they’re often describing a nervous-system shift, less tightness, fewer spikes of reactivity, or an easier time decompressing at the end of the day. That’s the context where many people try CBD for digestion, especially if symptoms seem stress-driven rather than purely food-triggered.
From a science standpoint, cannabinoids interact with the endocannabinoid system, which is involved in gut motility, sensation, and signaling. Clinical gastroenterology reviews describe cannabinoid activity in GI-related pathways, while also emphasizing that effects can vary and evidence depends on the specific condition and product.
It’s also important to know that CBD can cause side effects, including GI symptoms like diarrhea, and it can interact with medications. The NIH’s NCCIH notes side effects and cautions about interactions and possible liver-related concerns.
The FDA also warns that CBD can affect how other drugs work and may increase sedation when combined with other substances that slow the brain.
So if your symptoms feel like a stress-related stomach pattern, CBD is often framed as the “relaxation lever”, but it still deserves a safety-first approach.
Takeaway: CBD is commonly used when stress seems to drive gut sensitivity, but side effects and drug interactions are real considerations.
CBG (cannabigerol) is sometimes described as more “daytime-neutral” by consumers, and it’s frequently discussed in gut-wellness circles because research models highlight GI-related pathways tied to immune signaling and intestinal comfort.
Early research on CBG includes preclinical models (not definitive human proof). For example, animal-model studies have explored CBG-related effects in inflammatory pathways in the colon.
A broader 2024 review summarizes what’s known about CBG and repeatedly emphasizes that translation to humans and real-world products still needs more study.
Still, this “gut-pathways” emphasis is why many people gravitate to CBG for gut health when their goal is a steady, daytime-friendly approach, more “baseline support” than a bedtime unwind routine.
When people say they want gut balance, they usually mean one or more of these:
In research discussions, one theme is the role of the immune system and barrier function, especially when people talk about inflammation in the gut as a contributor to discomfort (again, not diagnosing, just describing a common concept). Reviews of cannabinoids and GI physiology discuss effects on motility, permeability, and inflammatory signaling, though clinical evidence varies by product and condition.
Also worth noting: CBG is generally described as non-intoxicating, and controlled research has examined whether it produces THC-like impairment (it does not appear to, in the way THC does).
Takeaway: CBG is often chosen for steadier daytime use and “gut-focused” support, but much of the gut-specific research is still preclinical or early-stage.
Most people comparing CBD and CBG aren’t trying to “treat a disease.” They’re trying to match the cannabinoid to the pattern they feel, stress-heavy versus gut-heavy, evening versus daytime, occasional versus daily.
One important frame: both compounds can influence GI-related signaling through the endocannabinoid system, and both have research gaps because commercial products vary widely (dose, format, purity, and added ingredients).
If you’re considering cannabinoid supplements, it helps to start with the “dominant driver” of your symptoms. Here’s a practical way people often think about it:
The point of this comparison isn’t to declare a winner, it’s to choose a hypothesis you can evaluate safely and calmly.
Takeaway: CBD is often framed as “stress-first,” while CBG is framed as “steady gut-first”, but evidence and product quality vary, so the smartest approach is structured and conservative.
Before you try anything new, it’s worth being very clear about the difference between wellness support and medical treatment, and about the fact that quality in the marketplace is inconsistent.
If you take prescription medications (especially those with “grapefruit warnings,” sedatives, seizure meds, or blood thinners), are pregnant or breastfeeding, have liver disease, or have complex medical conditions, it’s wise to talk with a clinician before using cannabinoid supplements.
Whether or not you ever use cannabinoids, the basics still move the needle, especially when symptoms fluctuate with stress. Because the gut-brain axis is bidirectional, routines that calm the nervous system can show up as better bowel regularity and less sensitivity over time.
If you’ve been told you have irritable bowel syndrome, major clinical resources commonly emphasize long-term management strategies like diet adjustments, stress management, and lifestyle changes.
Here are a few foundational moves many clinicians start with:
These steps aren’t flashy, but they create the conditions where any supplement choice, if you make one, can be evaluated more clearly.
Section takeaway: The most reliable gut support often starts with sleep, fiber strategy, and stress skills, because they work upstream of symptom flares.
It depends on the pattern. Many people consider CBD for digestion when they notice symptoms track with stress and tension, and they want a calming routine. Others consider CBG for gut health when they want steadier daytime support and a calmer baseline. Neither is guaranteed, and both should be approached cautiously with attention to product quality and interactions.
Yes. A stress-related stomach can show up quickly because stress hormones and nerve signals can change gut motility and sensitivity. Medical references discussing IBS describe stress-related increases in intestinal sensitivity and contractions.
Yes—the gut-brain axis is widely recognized in digestive health research and clinical discussions, especially for disorders of gut–brain interaction. It’s a framework for understanding why mood, stress, sleep, and digestion can affect each other.
If you suspect irritable bowel syndrome, it’s best to get evaluated first—especially if symptoms are new, severe, or changing. IBS is diagnosed based on symptom patterns and ruling out concerning causes; long-term management often includes diet, stress support, and (when needed) medical therapies.
Human evidence is limited. Interest in CBG partly comes from preclinical research exploring inflammatory pathways, which is why you’ll see it discussed alongside inflammation in the gut—but animal and lab findings don’t automatically translate into proven human outcomes.
CBD can cause side effects such as GI upset (including diarrhea) and can interact with medications. The NIH’s NCCIH and the FDA both emphasize safety concerns and the importance of considering drug interactions.
For cannabinoid supplements, look for third-party testing, a clear certificate of analysis (COA), and transparent labeling. Be cautious with products making disease claims—regulators have repeatedly stated that CBD products marketed to diagnose, treat, or prevent disease are not legally marketed as such.
If symptoms persist beyond a few weeks, disrupt daily life, or come with red flags (bleeding, weight loss, severe pain, persistent vomiting), it’s time for medical evaluation. That’s especially true if you’re unsure whether the pattern is IBS or something else.
CBD and CBG are often framed differently—CBD as a stress-to-body “downshift,” and CBG as a steadier daytime option. Whichever direction you’re curious about, build a safety-first plan, track patterns, and prioritize the fundamentals. That’s the most reliable way to protect your health while aiming for lasting digestive comfort.
Below are the primary references used to inform this article:

My name is Jake. I'm a certified health coach, accredited nutritionist, and I want to make health easier for everyone.
We have the 'most advanced healthcare' in history, yet millions are still sick and on more medication than ever. My goal is to make holistic health more achievable for everybody.
I read all comments, so please let me know what you think!
These statements have not been evaluated by the FDA. USA Medical products are not intended to diagnose, treat, cure, or prevent any disease. Please consult with a healthcare professional before use.

If you want steadier energy, more regular rhythms, and a

Save 50% on USA Medical CBG this week. Use code
If your goal is comfortable, consistent relief, not a rollercoaster,

If you’re wondering whether magnesium glycinate for sleep is worth
What we mean by IBD, IBS, and Crohn’s IBD is

USA Medical CBG Oil works quickly and keeps working for

In stock | Free shipping
In stock | Free shipping
In stock | Free shipping
In stock | Free shipping
In stock | Free shipping
In stock | Free shipping
In stock | Free shipping
In stock | Free shipping